All about Cervical Screening
We understand that screening can be daunting and lead to some difficult emotions. Here at the Middlewood Partnership we’ve created this blog to try and help prepare you and make the process less intimidating.
Cervical screening is not a test for cancer; it’s a test that checks the health of your cervix and helps find any abnormal changes before they can turn into cancer.
“Who will perform my cervical screening?”
We have a number of GPs and nurses across Bollington, Disley and Poynton who are trained to carry out cervical smears – it might make you more comfortable to know who you are seeing prior to your appointment. Our GPs can also complete the procedure at the same time, if you’re having a coil fitted at the practice.
|
|
|
|
|
|
|
|
|
|
|
|
“What equipment will be used?”
The plastic device used is called a speculum. They come in various sizes which we will tailor to each individual person.
Using lubrication on the tip of the speculum, it is inserted into the vaginal opening. Once inserted into the vagina, it is then gently opened so we can see your cervix. We then use the brush with the green stick to take a sample of the cells from your cervix. The brush is turned a total of 5 times whilst resting on your cervix.

“What do I need to do?”
The main thing you can do is to turn up. We understand that these appointments can be worrying for some, so here are a few tips that can help:
- Wear something comfortable and easy to remove; a loose skirt or dress you can lift is ideal.
- There is no need to prepare the area by shaving/waxing.
- Avoid booking an appointment around the time of your period, as there is a higher chance of an inadequate sample.
If you have any concerns about having a smear test, please share these with us so we can make a plan to support you having this test.
“What are you looking for exactly?”
Cervical screening checks a sample of cells from your cervix for certain types of human papillomavirus (HPV).
Human Papillomavirus (HPV) – The Facts:
- HPV is a common virus with some strains causing warts and verrucae.
- Most people will encounter it at some point in their lives and never be aware of it.
- There are more than 100 types of HPV.
- High-risk HPV – strains that increase your risk of certain types of cancer, like cervical cancer.
- HPV spreads from any type of sexual contact, including close skin-to-skin genital contact and sharing sex toys.
- Condoms do not offer full protection from the virus.
- The immune system in most cases gets rid of the virus. For some however, this does not happen, and over time the virus can damage cells in the body and increase the likelihood of certain cancers.
.
Reducing your risk of HPV:
- The NHS offers children aged 12-13 the HPV vaccine.
- Using a barrier method of contraception like condoms can lower your risk of contracting HPV.
- Smoking increases the risk of getting HPV and developing HPV related cancers.
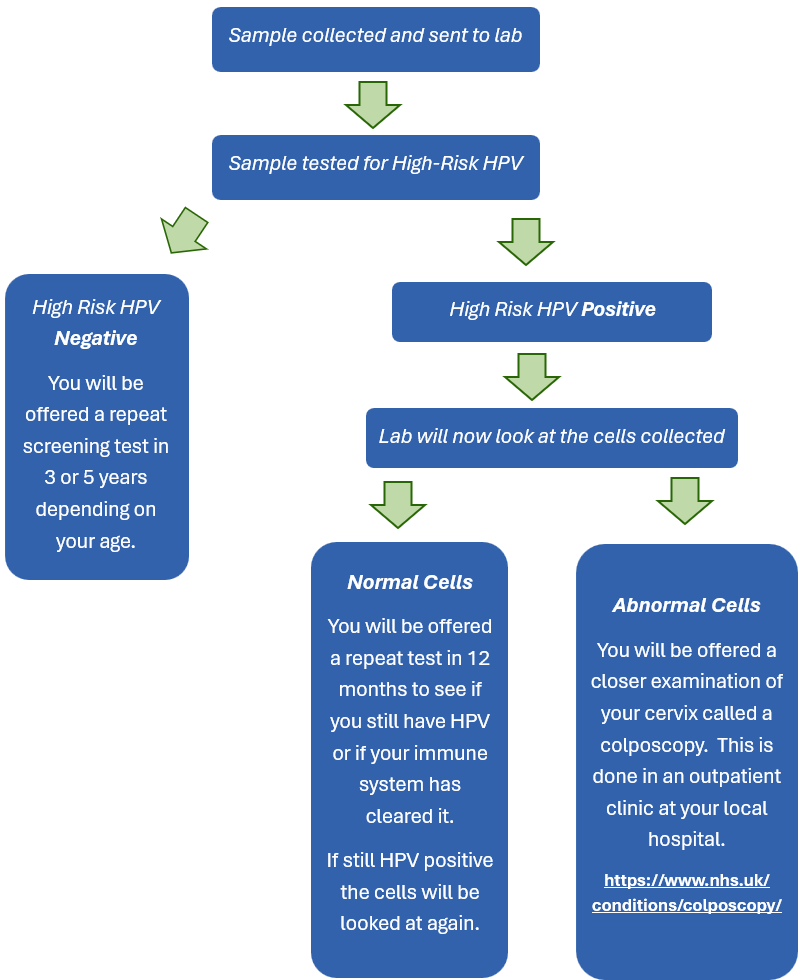
“How does it work in the background?”
“I don’t think I need a cervical screening because…”
While there’s a lot of helpful information available, there’s also a lot of myths or misconceptions about cervical screening appointments too – we’ve tackled some of the most common ones below:
.
- Myth – “I don’t need one because I have had the HPV vaccine”
Reality – Although this will lower your risk the vaccine does not cover every strain of HPV.
.
- Myth – “I don’t need one because I have never had sex”
Reality – HPV can be transmitted without having sex. This includes close skin-to-skin contact of the genitals, sharing sex toys, transferring fluids on hands and fingers and oral sex.
.
- Myth – “I don’t need one because I am lesbian or bisexual”
Reality – Although HPV is more easily passed through sex with men, it can still be spread in other ways. This includes close skin-to-skin contact of the genitals, sharing sex toys, transferring vaginal fluids on hands and fingers and oral sex.
.
- Myth – “I don’t need one because I am transgender or non-binary”
Reality – If you still have a cervix, you are at risk. If you have had a total hysterectomy and removal of your cervix, you do not need cervical screening.
“But, but, but…”
We appreciate that this test can be very difficult for some people and lead to some uncomfortable emotions. We hear about a lot of things that people see as barriers to getting their screening, but there are things we can do to help.
.
- “I’m worried about the pain,” or “I’m too embarrassed.”
You can book an appointment with a GP or nurse to discuss your concerns. We would be happy to show you the equipment used.
.
- “I’m too busy to come.”
We offer early morning and Saturday appointments as part of our Extended Access service if work commitments make it hard for you attend.
.
- “There will be a language barrier.”
We have access to Language Line if English is not your first language, and you are worried you may not understand what is said during your appointment. Please make us aware when booking if this is something you need.
.
- “I’m worried about how it will affect my mental health / sexual trauma.”
If you have mental health difficulties or have been sexually assaulted or abused, there are a number of services available that can offer support:
https://www.rapecentre.org.uk/
https://www.thebiglifegroup.com/service/talking-therapies-eastern-cheshire/
.
- “It will be too difficlut with my physical disability.”
If you have a physical disability – please talk to us about any adjustments we can make to help during the appointment.
-
- Feel free to ask for a chaperone, bring a friend for support or to listen to music or a podcast during the examination.
- Remember YOU are in control! We will take the appointment at your pace, ensuring you are comfortable during the examination. You can say STOP at any point.
